Frequently Asked Questions
What is Bariatric Medicine?
Bariatric Medicine is the medical specialty that deals specifically with the treatment and care of overweight and obese individuals and their related medical conditions. Physicians who become board certified in Bariatric Medicine have specialized education, training, and experience, and have had to pass both rigorous written and oral examinations. Medical Bariatrician’s are uniquely prepared to treat the conditions of overweight and obesity.
Is your program affordable?
Our program is very affordable. We are always open and up front about costs – nothing is hidden and there are no contracts to sign. Overweight, obesity, and their related illnesses are enormously expensive. Becoming healthy has its costs like any other product or service but being unhealthy or developing a chronic disease has an even greater cost. Prevention or early reversal of disease is enormously more economical than intervention and treatment of disease. The best time to fix a problem 5 or 10 years from now is today. For an exact quote on our individualized weight loss program, call us to schedule a free consultation.
Are program costs covered by insurance?
Health insurance does not always cover medically-supervised obesity and weight loss treatments and we do not bill insurance for our services. Most people can use their Flexible Spending or Health Savings Account for these services. In addition, your treatment costs may be tax deductible.
What if I only need to lose 10-15 pounds?
Whether you need to lose 10 pounds or 110 pounds, we can help you reach your weight loss goals. We will develop a customized program that can help you lose weight and transition into a healthier lifestyle. To see if you need to lose weight, click here to view our BMI chart (or waist circumference chart, etc.)
Will I be hungry on this program?
No, not at all. Many patients actually report reduced hunger and increased energy.
I have diabetes can I be on the program?
Yes. Our program is physician-supervised. Patients suffering from medical conditions, including diabetes, can be treated with your doctor’s permission. Our program can help you control or even reverse some medical conditions so that you may be able to come off of some of your medication.
How often do I have to visit the clinic?
It differs depending on your program, your medication (if used) and your weight loss phase. During the Active Phase, you will generally visit the clinic on a weekly basis initially. Once you have demonstrated understanding of the principles we teach and have demonstrated weight loss success, you will visit us on a monthly basis until you reach your weight loss goal.
Can I do this program with my Primary Care Physician?
I recently had my physical, EKG, and blood work done. Do I need to repeat the exams at the initial consultation?
Recent physicals or tests conducted by your Primary Care Physician within the past three months are acceptable. In order for us to retrieve this information, you will be asked to sign a release form during your first visit.
What type of food do I eat while on the program?
To teach you how to be successful for the long term, we provide education that promotes real food that you can obtain from grocery stores and farmers markets. We do offer physician-grade meal replacements, protein shakes and supplements for convenience and structure along with a variety of other tools to help you reach your goal.
Hemoglobin A1C: What is it? Why should you care?
Type 2 diabetes accounts for 90-95% of all cases of diabetes.1 Often times, there can be a long period of time between when diabetes develops and obvious symptoms become present. Early detection of disease is crucial to prevent the progression from prediabetes to diabetes, or to reduce the risk of complications of diabetes. Long term complications of diabetes include cardiovascular disease such as heart attack and stroke, nerve, kidney, eye, and foot damage, bacterial and fungal skin infections, hearing impairment, and Alzheimer's disease.
Am I at risk? Should I get tested?
Testing for diabetes should be considered in adults of any age who are overweight or obese (BMI > 25 kg/m2) who also have one or more of the following additional risk factors:
- 1st degree relative with diabetes
- Physical inactivity
- High blood pressure (>140/90 mmHg or on medication for hypertension)
- Abnormal cholesterol or triglyceride results: HDL ("good" cholesterol) <35 mg/dL or triglyceride (fat in the bloodstream) levels >250 mg/dL
- High risk race/ethnicity: African American, Latino, Native American, Asian American, Pacific Islander
- Women with polycystic ovarian syndrome
- Women who delivered a baby weighing >9 lbs or were diagnosed with gestational diabetes
Additionally, testing should begin at age 45 for ALL patients, regardless of BMI. Being overweight is strongly linked to the development of type 2 diabetes, but not everyone with type 2 diabetes is overweight.
What test should I be asking for?
Hemoglobin A1C (HbA1c, glycosylated hemoglobin) is a blood test used to measure the average blood sugar level over the previous 2-3 months. Sugar molecules in the bloodstream react with hemoglobin (the protein that carries oxygen) in the red blood cells, forming a new molecular compound on the surface of the cell. The rate at which these new compounds form is directionally proportional to the amount of sugar in the blood stream; i.e. the higher the blood sugar levels, the more of these compounds are formed, and the higher the HbA1c result.
A HbA1C result less than 5.7% is normal. A result of 5.7-6.4% indicates that you are pre-diabetic and are at an increased risk for developing full blown diabetes. A result of 6.5% or higher is considered diabetic.
Without weight loss, up to 30% of people with pre-diabetes will develop type 2 diabetes within 5 years.3 If you're overweight, losing just 5% of your body weight will dramatically decrease your risk.
Our program is designed to reduce your risk of diabetes. Or, if you have already developed diabetes, we help patients achieve better HbA1c control on less medication and many times can even reverse diabetes..
Call us today at (706) 922-1717 or contact us online if you would like help.
What is the truth about cholesterol and heart disease?
Cholesterol, Saturated Fat, & Heart Disease
We’ve been told that saturated fat is unhealthy and is claimed to be the cause of heart disease putting us at an increased risk of dying from a heart attack or stroke. Foods that are high in saturated fat include lard, butter, cream, fatty meats, coconuts, and other full-fat dairy products.
In 1913, researchers suspected that eating saturated fat correlated with increased levels of cholesterol in the bloodstream. There were also some studies that tried to link high levels of cholesterol with increased risk of heart disease. Therefore, it was assumed that eating saturated fat increased your risk of dying from a heart attack or stroke. This was the basis of the “diet-heart hypothesis” and became part of the FDA dietary guidelines which recommended low-fat and higher carb diets before it was ever truly tested and proven. Since that time, obesity has tripled, heart disease has tripled, and diabetes has tripled. The case against saturated fat was pieced together with observational data, short-term trials, animal studies, and guesswork, all showing correlation and none of which proved causation.
Clarifying Cholesterol
The word “cholesterol” is often used inaccurately and most of us have an oversimplified understanding of what it is really doing in our body. For starters, the term “good cholesterol” (HDL) and “bad cholesterol” (LDL) are woefully misleading as these aren’t actually cholesterol at all, they are the proteins that carry cholesterol around in the bloodstream. HDL stands for High Density Lipoprotein and is shown to be protective against heart disease. LDL stands for Low Density Lipoprotein and has been linked to increased risk of heart disease.
It sounds logical that if you ate saturated fat, you would increase LDL levels, and therefore, increase your risk of heart disease. However, there several flaws surrounding this logic. The first fact that has been mostly ignored is that saturated fat also increases HDL (good) cholesterol. The second problem with this logic is seen in new research showing different subtypes of LDL, some of which are bad and others not so bad. There are very small dense LDL that definitely drive heart disease by penetrating arterial walls easily during a state of inflammation and starting a plaque formation which can in turn cause a heart attack or stroke. The other type of LDL is a large, buoyant particle that is too fluffy to penetrate the arteries and start a plaque formation. This type of LDL is neither good nor bad, and does not increase your risk of heart disease. The most interesting piece of information that comes from all of this is the fact that yes, eating saturated fat increases HDL and LDL, however it changes the LDL particles from the small, dangerous form to the large, neutral form. So, even though saturated fat can increase LDL, they are changing the subtype from the particles that are associated with heart disease to the particles that reduce your overall risk.
The supposedly harmful effects of saturated fat continue to be the cornerstone of modern “low fat” dietary guidelines even though multiple studies have found that there is no link between saturated fat consumption and heart disease. One review of 21 studies, with a total of 347,747 participants, published in 2010 concluded that there is absolutely no association between saturated fat and heart disease. Another review published in 2014, looked at 76 studies, totaling 643,226 participants and again concluded no link between saturated fat and heart disease. On the other hand, there have been many other studies confirming the modern “low-fat” diet being preached provides no benefit for heart disease or death. On top of that, the studies that replaced saturated fat with vegetable oils actually show an increased risk.
Cholesterol isn’t all bad. We need cholesterol for many important functions in our body. It is the basic building block for all our cells. It is crucial for synthesizing vitamin D and sex hormones like estrogen and testosterone and critically important for our immune system. It works to build cell membranes and produce bile acid to help digest food. Cholesterol isn’t the bad guy, as long as you have the right kind.
Despite thousands of scientists, decades of work and billions of dollars spent, the “diet-heart hypothesis” still has not been supported by any high quality study. The saturated fat myth was never proven in the past, has not been proven today, and will never be proven because saturated fat simply does not increase your risk of heart disease.
References:
Adele H. Hite, M.A.T., Richard David Feinman, Ph.D., Gabriel E. Guzman, Ph.D., Morton Satin, M.Sc., Pamela A. Schoenfeld, R.D., Richard J. Wood, PhD., “In the face of contradictory evidence: Report of the dietary guidelines for Americans committee,” Nutrition. 26(10), 2010, 915-924.
Chowdhury, R., Warnakula, S., Kunutsor, S., et al., “Association of dietary, circulating, and supplement fatty acids with coronary risk: A systematic review and meta-analysis.” Annals of Internal Medicine. 160(6), 2014.
Gunnars, Kris., “Saturated fat: good or bad?” http://authoritynutrition.com/saturated-fat-good-or-bad.
H Campose, JJ Genest Jr, E Blijlevens, J R McNamara, J L Jenner, J M Ordovas, P W Wilson, E J Schaefer. “Low density lipoprotein particle size and coronary artery disease.” Arteriosclerosis, thrombosis, and vascular biology. 12, 1992, 187-195.
Minger, Denise., “Death by food pyramid.” (2013), Primal Blueprint Publishing; Malibu, CA.
Siri-Tarino, P. W., Sun, Qi, Hu, Frank B., and Krauss, Ronald M., “Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease.” The American Journal of Clinical Nutrition. 102(2), 2015.
Weinberg, Sylvan Lee., “The diet-heart hypothesis: a critique.” Journal of the American College of Cardiology. 43(5), 2004, 731-733.
Why Choose an Obesity Medicine Specialist?
Let's face it. When it comes to weight loss, the government-recommended dietary guidelines have clearly failed us.
Americans have been hearing "eat less, exercise more" for over 50 years, yet the rates of obesity and chronic disease continue to skyrocket. Our program is backed by a growing amount of medical research that challenges these outdated guidelines. We're attacking the obesity epidemic at the source using a comprehensive, individualized approaches that focuses on eating real food and addresses the underlying cause of weight gain.
With more than 30 years of experience working in obstetrics and gynecology, endocrinology, and preventive medicine, I have seen first-hand how our current system is failing us. I became interested in obesity medicine because I saw how being overweight can negatively affect every part of our health and quality of life. Just treating overweight and obesity can have enormous health benefits far beyond just looking and feeling great
Why do I need follow-up visits?
Weight Loss Success: The Importance of Follow-Up Visits
If I learned the nutritional guidelines for weight loss at my first visit, why do I need to keep coming back?
The success of independent weight management after formal weight loss programs end is unfortunately low. Studies have shown that patients in treatment longer than 6 months tend to see greater weight loss success compared to those in treatment less than 6 months. The American Medical Association now recognizes obesity as a chronic disease, and at Advanced Medical Weight Loss of Augusta, we strongly believe chronic diseases like overweight, obesity, and type II diabetes should be treated just as other chronic diseases are such as hypertension, diabetes, hypothyroidism, and asthma.
Most importantly, follow-up visits are used to track weight loss to make sure you are losing weight in a safe and healthy manner. We not only track your weight, but also monitor blood pressure, biometric measurements, body composition, and laboratory blood results. At every visit, we continue to build on the medical and nutritional education provided in your first visit to increase your knowledge of medical science and give you knowledge and tools to successfully lose weight and also maintain that weight loss.
Follow-up visits are also crucial in managing any existing medications or weight loss medications used as part of our program. Many patients are able to decrease the amount or even eliminate some current medications they are taking. Most common are medications for managing conditions such as high blood pressure, high cholesterol, and diabetes. If you are utilizing any of the medications specific to our program, our physician uses follow-up visits to monitor these as well and make any changes if necessary.
This combination of individualized weight loss plans along with scheduled follow-up visits, is designed to give you the knowledge and know-how needed for maximum weight loss and successful maintenance. To learn more about our program or to schedule your first appointment, call 706-922-1717 or contact us online.
Why do you recommend I have a primary care physician?
Our entire team is specialized in the treatment of weight management, and we consider losing weight to be a preventative health measure for many of our patients. While treating your obesity will often involve the treatment of other diseases that are related to your weight, there are many other health issues that do not fall under this category. As a result, it is important to have a primary care physician that you can contact if needed while participating in our medical weight loss program.
The field of bariatrics or medical weight loss is a specialty. Your primary care physician may have knowledge about the importance of losing weight, but it is not the main focus of their practice. When you are trying to lose weight, having a team of Weight Loss Specialists is crucial for the education, specialized weight loss knowledge, support, motivation, and encouragement you will need.
Many patients that struggle with obesity have already developed serious conditions such as diabetes or heart disease; and therefore, already have a primary care provider. We will work with your doctor to help you to become even healthier. Your primary physician will continue to be responsible for regular screenings for other conditions that you may need addressed.
Will insurance cover my visits?
At this time, we do not file through insurance because insurance companies do not consider this a covered benefit. However, we keep our fees very reasonable and most people consider this a valuable investment in their health and longevity. Patients have been able to utilize Flex Spending Accounts and HSAs, if you have that available to you.
How do I Avoid the Holiday Weight Gain
Holidays are a busy time, with seemingly endless opportunities to eat. Family gatherings, office parties, holiday and end-of-semester programs at our children's schools, treat samples handed out as we shop, and countless aisles of holiday candy. Here are a few strategies you can use to help avoid the holiday weight gain:
- Focus on maintaining your current weight. Challenging yourself to lose weight over the holidays is setting yourself up for failure. Think about all the hard work you have put into accomplishing your goals at this point and use that as motivation.
- Don't gorge on any special holiday food but don't deprive yourself of anything you want to taste. Try to be mindful what are eating and savor each bite care.
- Avoid the trap of thinking you can eat what you want because you can just start over. There will always be holidays, birthdays, and multiple occasions to splurge. But just remember that nothing tastes as good as thin feels.
- Exercise is critically important for good health but unless you are an elite athlete, to be extremely difficult to exercise off holiday overindulgence
- Keep tabs on yourself. Be mindful of what you are eating, weigh yourself at least weekly, and try on your favorite clothes to make sure they still fit.
- Remember all the reasons why reaching and maintaining your healthy weight is important to you.
What is insulin resistance and does it cause weight gain?
Insulin is the hormone that signals cells to absorb excess glucose from the bloodstream and store it as fat. In insulin resistance, cells do not respond properly to insulin, and the pancreas has to release more and more of the hormone to get glucose out of the blood. Over time, the pancreas fails to produce enough insulin to overcome this cellular resistance, leading to increased blood glucose levels (pre-diabetes, diabetes).
Do I have insulin resistance? Insulin resistance can be present for years before any symptoms of high blood sugar appear. Knowing the signs of insulin resistance, and addressing it early on, can help prevent many of the health problems associated with this condition.
Here are some signs you may have insulin resistance:
- skin tags
- acanthosis nigricans: darkening around skin creases, especially around the neck, armpits, or groin
- overweight
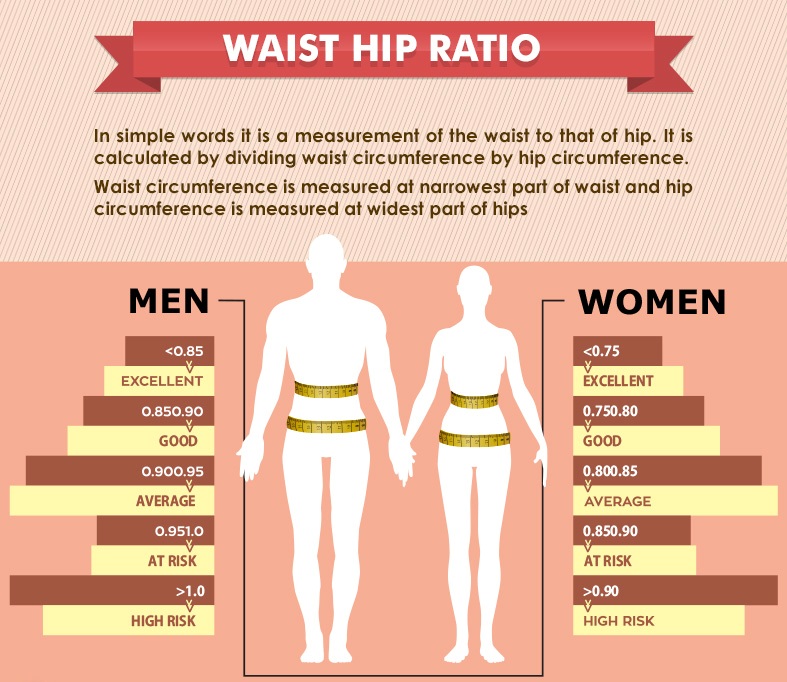
- increased waist measurement: >35 inches for women, >40 inches for men
- increased waist to hip ratio: >0.8 women, >1 men (see chart below)
- high blood pressure
- borderline or high blood sugar (A1c > 5.6%)
- high blood triglycerides
- low HDL (good) cholesterol
- elevated liver enzymes (ALP, AST, ALT)

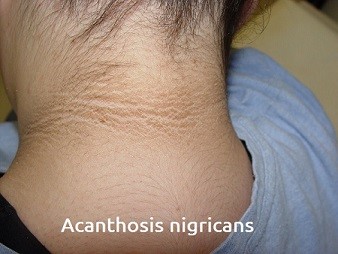
Insulin resistance is a major contributor to weight gain, type 2 diabetes, and many other health problems. Treating the underlying cause, whether it's insulin and/or other hormone irregularities, is critical to weight loss success.
Does your current weight loss program address these issues?
If not, contact Advanced Medical Weight Loss of Augusta to get started. Call 706-922-1717.
What is insulin resistance and why is it important?
Insulin Resistance is a metabolic condition that increases the chances of developing type 2 diabetes, heart disease, and stroke, and obesity.
Insulin is the hormone that regulates the amount of blood sugar in your bloodstream. Insulin is the hormone that transports glucose from the blood stream into cells. Insulin transports sugar or glucose out of the blood stream into all cells including fat, muscle, and liver cells to be stored or used as energy.
High levels of insulin over a long period of time will create a condition called Insulin Resistance. When someone develops Insulin Resistance, their fat, muscle, and liver cells do not respond to normal levels of insulin and the body is forced to make more insulin just to move the same amount of sugar. You can think of these cells as being "resistant" to insulin's job, and therefore insulin is less effective. Since insulin is a fat storing, a fat building, and a fat locking hormone, higher levels of insulin due to insulin resistance eventually will create both overweight and obesity. If this process continues without interruption and blood sugar levels are not controlled, the pancreas, which produces insulin, will no longer be able to keep up with the needed production and eventually type-2 diabetes will develop.

Infographics www.cdc.gov
Is obesity a disease?
besity has always been poorly understood within traditional healthcare. It was generally thought that the solution to Obesity was to eat less and burn more calories, and that the inability to achieve desired results was related to laziness and undisciplined behavior. The blame was placed back onto the patient. The message was “if you’re fat, it’s your fault.” This statement is 100% false, however it is still commonly the message we hear today.
 The American Medical Association issued a statement in 2013 that classifies Obesity as an actual disease….. Not because of laziness and undisciplined behavior.
The American Medical Association issued a statement in 2013 that classifies Obesity as an actual disease….. Not because of laziness and undisciplined behavior.
The Obesity Medicine Association defines Obesity as: “a chronic, relapsing, multi-factorial, neurobehavioral disease, wherein an increase in body fat promotes adipose tissue dysfunction and abnormal fat mass physical forces, resulting in adverse metabolic, biomechanical, and psychosocial health consequences.”
What is the definition of a disease? The American Medical Association proposes that a disease must have the 3 following characteristics:
- An impairment of the functioning of some aspect of the body
- Demonstrates characteristic signs and symptoms
- Causes harm and morbidity
Does Obesity Fit the Definition of a Disease?
1. Impairment of the function of some aspect of the body:
The intake of food is regulated by specific hormonal signals sent and received by the brain, as well as signals from the body, including the gut, the pancreas, and the fat tissue. This balance helps to regulate the feelings of hunger and satiety, and allows for body weight regulation.
Studies show that the Hedonic Pathway, or Reward System”, can override the brain’s regulatory system for food intake and energy balance. Certain foods in our environment are acting in some ways like a hormone that serves to reset the body’s target weight I call the Body Weight Set Point.
There is also impairments with insulin sensitivity and hyperinsulinemia. Insulin is a hormone that regulates the amount of blood sugar or glucose in your bloodstream. Insulin moves sugar out of the blood stream into fat, muscle, and liver cells to be stored or used as energy. High insulin levels promote excessive storage of fat in the liver and muscle as well as fat cells promoting weight gain.
2. Characteristic Signs and Symptoms:
Obesity is characterized by excessive adipose (fat) tissue and can manifest as increased BMI, increased waist circumference, and/or increased body fat percentage.
3. Harm and Morbidity:
Obesity can be associated with medical conditions, which many tend to improve with weight loss.
- Increased inflammation
- Metabolic syndrome
- Diabetes
- High blood pressure
- High cholesterol
- Heart disease
- Stroke
- Obstructive sleep apnea
- Osteoarthritis
- Gallbladder disease
- Fatty liver disease
- Polycystic ovarian syndrome
- Infertility
- Renal failure
- Cancer
- Depression
Want a program to address the underlying issues to obesity? Call us today and make an appointment to take control of your health! Advanced Medical Weight Loss of Augusta 706 ) 922-1717.
Is Type 2 Diabetes just about blood sugar?
 Insulin Resistance is a metabolic condition that increases the chances of developing weight gain, obesity, type 2 diabetes, heart disease, and stroke just to name a few.
Insulin Resistance is a metabolic condition that increases the chances of developing weight gain, obesity, type 2 diabetes, heart disease, and stroke just to name a few.
Insulin is a hormone that regulates the amount of blood sugar called glucose that is in your bloodstream. Insulin is the hormone that transports blood glucose out of the blood stream into cells
When someone has Insulin Resistance, their fat, muscle, and liver cells do not respond to normal levels of insulin and the body has to make more insulin just to move the same amount of glucose. You can think of these cells as being "resistant" to insulin's job, and therefore insulin is less effective. If this process continues without interruption and blood sugar levels are not controlled, then overweight, obesity, and type-2 diabetes will develop.
The number of people with diabetes is increasing rapidly, with no end in sight. One-third of adults don’t know they have diabetes, and it is estimated that 90% of pre-diabetics are unaware they are effected.
Current guidelines are failing to address this growing issue and continue to offer a Band-Aid approach to care. It is assumed that once someone is diagnosed with Traditionally Type 2 Diabetes has been considered a chronic progressive disease because we have traditionally just focused on blood sugar. We begin with lifestyle changes along with diet and exercise and when that no longer controls the blood sugars, physicians prescribe medications that promote one’s pancreas to produce more insulin. When this is no longer adequate because the blood sugars become more elevated, insulin injections are then prescribed while all the time the condition progressively gets worse. With type II diabetes, which is really insulin resistance, focusing just on blood sugar turns out to be a big mistake because the disease is continuing to get worse at the cellular level.
The more insulin your body is exposed to, the more Insulin Resistant you become, making it more and more difficult to control blood sugar. If someone already has high insulin, how does giving them more insulin “fix” the problem? It doesn’t. Blood sugar will temporarily be controlled but eventually the body adapts to the higher insulin levels and more medication is needed. We are chasing the symptom which is the blood sugar and ignoring the true cause of Type II Diabetes which is high levels of insulin and insulin resistance. This is the problem with our modern day management of Type 2 Diabetes in our health care system today.
Managing high blood sugar alone does little for the overall management of Diabetes. The ultimate goal should be reversing the underlying cause: Insulin Resistance…. which just so happens to also lower blood sugar. Treating the Insulin Resistance will reduce the amount of medication needed and eventually return the body to a more normal insulin response.
What do I do to get started losing weight?
You probably have many questions about our programs and which one would be best for you. You may be concerned about the costs involved, how a weight loss program will interfere with your schedule, or whether a medical weight loss program is the best option for you.
To answer your questions we invite you to meet with our program administrator for an informal information session. The information session is not a sales pitch. You do not need to decide anything on the spot and we will give you information to take with you so you can look it over at home. Depending on how many questions you have, an information session takes about an hour.
Keep in mind there are no enrollment fees and no required long term contracts. The mission of Dr. Paul Thaxton and the entire staff of Advanced Medical Weight Loss Augusta is to help you become healthier.
We understand people become overweight for a variety of biological, cultural, and emotional reasons. Therefore, we put the expertise of an experienced, caring, and highly skilled medical weight loss team at your fingertips.